Need Cialis covered by BCBSNC? Confirm your prescription’s details with your doctor. Then, carefully review BCBSNC’s formulary to ensure Cialis is covered under your specific plan. This step prevents unexpected out-of-pocket costs.
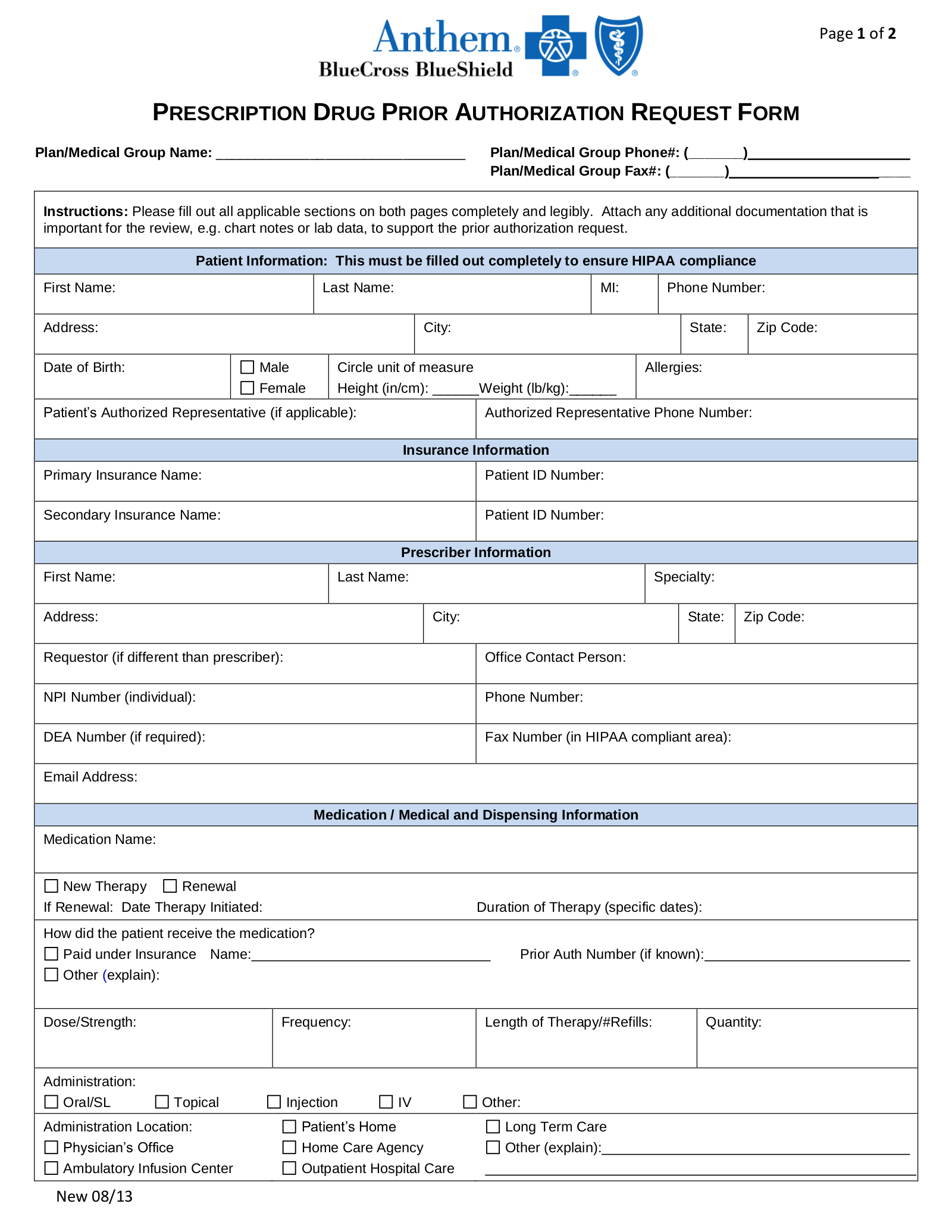
Next, gather necessary documentation. This typically includes your prescription, a completed prior authorization form (obtainable from BCBSNC or your doctor), and any relevant medical records supporting the need for Cialis. Incomplete applications cause delays. Submit your application directly to BCBSNC using their online portal or fax number, clearly indicating your member ID.
BCBSNC generally processes applications within 7-10 business days. However, complex cases may require more time. Track your application’s status online or by phone. If your application is denied, immediately request a reconsideration and provide any additional supporting medical information. Always maintain clear communication with BCBSNC and your doctor throughout the process.
- BCBSNC Prior Authorization for Cialis: A Comprehensive Guide
- Required Documentation
- Expediting the Process
- Potential Reasons for Denial
- Appealing a Denial
- Alternative Treatments
- Disclaimer
- Understanding BCBSNC’s Prior Authorization Requirements for Cialis
- Navigating the Prior Authorization Process with BCBSNC for Cialis
- Understanding BCBSNC’s Requirements
- Tips for a Smooth Process
- Appealing a Denial
- Contact Information
- Tips and Strategies for a Successful Cialis Prior Authorization with BCBSNC
BCBSNC Prior Authorization for Cialis: A Comprehensive Guide
Contact your BCBSNC provider directly to confirm current requirements. Their phone number and online portal are your best resources for the most up-to-date information.
Required Documentation
Generally, expect to provide the following:
- Prescription from your doctor
- Patient demographics
- Medical necessity documentation detailing the need for Cialis (this might include clinical notes, lab results, etc.). Be sure to clearly state the diagnosis and its connection to Cialis use.
- Prior authorization form (downloadable from the BCBSNC website).
Failure to submit complete documentation will likely result in delays.
Expediting the Process
- Submit your prior authorization request electronically through the BCBSNC provider portal whenever possible. This often speeds up processing.
- Ensure your doctor clearly details the medical necessity for Cialis in their documentation. Vague or insufficient justification can lead to denial.
- Follow up on your submission status. Contact BCBSNC if you haven’t heard back within a reasonable timeframe, which varies but often is a few business days. Have your claim number readily available.
Potential Reasons for Denial
Common reasons for denial include:
- Incomplete or missing documentation
- Lack of medical necessity clearly stated by your physician
- Prescription not meeting BCBSNC formulary requirements
- Prior authorization not completed correctly
Appealing a Denial
If your prior authorization request is denied, carefully review the denial reason and follow the instructions provided for filing an appeal. Gather any additional documentation that might strengthen your case. Act quickly; there are usually time limits for appeals.
Alternative Treatments
If Cialis is denied, discuss alternative treatment options with your doctor. They can help explore other medications or therapies to manage your condition.
Disclaimer
This guide provides general information. Always consult your doctor and BCBSNC directly for the most accurate and up-to-date information regarding prior authorization procedures.
Understanding BCBSNC’s Prior Authorization Requirements for Cialis
Check BCBSNC’s online provider portal for the most up-to-date requirements. This portal contains the specific criteria for Cialis prior authorization, including diagnosis codes and supporting documentation needed.
Generally, expect to provide medical records demonstrating a diagnosis requiring Cialis treatment. These records should clearly link your patient’s condition to the need for this medication. Include detailed information about previous treatment attempts and their outcomes.
Be sure to accurately complete the prior authorization form. Inaccurate or incomplete forms often lead to delays. Pay close attention to all fields, ensuring complete and correct information regarding the patient, the prescription, and the diagnosis.
Contact BCBSNC’s provider services directly if you encounter difficulties or have questions about their requirements. Their phone number and contact information are readily available on their website.
Familiarize yourself with the appeals process. Understand the steps involved if your prior authorization request is denied. Having this knowledge ensures a smoother process should a denial occur.
Remember, policies change. Regularly review the BCBSNC website for updates to their prior authorization guidelines for Cialis to maintain compliance.
Navigating the Prior Authorization Process with BCBSNC for Cialis
First, gather all necessary information: your prescription, doctor’s contact information, and your BCBSNC member ID. This significantly streamlines the process.
Understanding BCBSNC’s Requirements
BCBSNC often requires documentation supporting the medical necessity of Cialis. This usually involves details about your medical history, particularly conditions like erectile dysfunction or benign prostatic hyperplasia (BPH). Ensure your physician provides clear and concise medical rationale. Specific diagnostic codes are helpful; check BCBSNC’s website for the latest codes.
Submit your prior authorization request through the BCBSNC provider portal. This online method is generally quicker than fax or mail. Familiarize yourself with the portal’s interface beforehand.
Tips for a Smooth Process
Follow up. After submitting your request, follow up with BCBSNC within a week if you haven’t received an update. A polite inquiry can prevent delays. Check your online account for the status.
Be prepared for potential questions. BCBSNC may request additional information. Respond promptly and completely. A timely response accelerates the approval process.
Appealing a Denial
If your prior authorization is denied, carefully review the denial letter. It usually outlines reasons for the denial. If you disagree, prepare a detailed appeal with supporting medical documentation. Clearly address the reasons for denial in your appeal letter. The appeal process is clearly detailed on the BCBSNC website.
Contact Information
For assistance with prior authorizations, consult the BCBSNC member services number listed on your insurance card or their website. They can provide clarification on their requirements and the status of your request.
Tips and Strategies for a Successful Cialis Prior Authorization with BCBSNC
Gather all necessary information upfront. This includes your prescription, doctor’s notes detailing your medical history and the rationale for Cialis, and any relevant lab results. Missing information delays the process.
Use BCBSNC’s online portal. Submitting your prior authorization request electronically is faster and provides tracking capabilities. You can monitor the status of your request and identify any missing information.
Clearly articulate the medical necessity. Your physician’s supporting documentation should explicitly state why Cialis is the most appropriate treatment for your specific condition, considering alternatives and potential risks/benefits.
Follow BCBSNC’s specific guidelines. Carefully review their prior authorization forms and instructions. Incomplete or incorrectly filled forms lead to rejection.
Maintain consistent communication. If you encounter delays, contact BCBSNC directly to inquire about the status of your request. Provide any additional information requested promptly.
Consider alternative medications. If Cialis is denied, discuss alternative treatment options with your doctor. They might suggest medications with a higher approval rate.
Appeal a denial. If your prior authorization is denied, review the reason for denial and consider submitting an appeal with additional supporting documentation.
Contact a BCBSNC representative. If you’re struggling with the process, a direct conversation may clarify requirements and expedite the authorization.